Dr. Steven Goldman is the C. Leonard Pfeiffer Chair in Cardiovascular Medicine at the University of Arizona (UA). Dr. Goldman received his undergraduate education at Cornell University, his medical degree from the University of Cincinnati, his residency training at the University of Illinois, the University of Chicago and Stanford University and his cardiology training at Pacific Medical Center in San Francisco. He is a Vietnam veteran serving with the Marine Corps in Da Nang in 1970-71. In 1975, he came to the UA and the Tucson VA where he was Chief of Cardiology for 35 years. At the VA, he was the Principal Investigator (PI) on four large multi-center trials on the treatment of heart failure and graft patency after coronary artery bypass surgery.
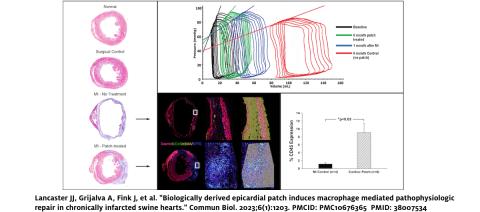
Dr. Goldman's laboratory has a long history studying the pathophysiology of heart failure and exploring new treatments for heart failure. In the past, he and Dr. Eugene Morkin developed a thyroid hormone analog to treat heart failure. His lab is currently working with induced pluripotent stem cells derived-cardiomyocytes (iPSC-CMs) based on the 2012 Nobel Prize winning technology developed by John Gurdon and Shinya Yamanaka. Dr. Goldman's lab was one of the first groups in the world to use iPSC-CMs for heart disease; they have effectively treated heart failure in preclinical animal models of disease. Dr. Goldman and Jordan Lancaster PhD co-founded a UA biotech spin-off company, Avery Therapeutics, to commercialize this work. Together with Dr. Jen Koevary, they are in discussions with the FDA to proceed with a clinical trial designed to create new heart muscle in patients with damaged hearts.
In addition to this laboratory work, Dr. Goldman has studied graft patency after coronary artery bypass grafting (CABG). Dr. Goldman has been the PI on a number of large multi-center trials to examine graft patency and new treatments for heart failure. These studies resulted in our group defining graft patency up to 10-years after CABG for each branch of the coronary artery grafted. The therapeutic findings of these studies are: 1) the major determinant of graft patency after CABG is the size of the recipient grafted coronary artery, 2) giving aspirin via a nasogastric tube 6 hours after CABG improves graft patency. The use of aspirin after CABG is now standard therapy world-wide because of this work. Dr. Goldman is currently the PI on the long-term 10 year follow up trial of radial artery patency after CABG.
Please see the Publications page for the most important manuscripts to come out of Dr. Goldman's laboratory.
Here is a video of our beating patch (https://youtu.be/_GnREeMiKAo).
|
IN THE NEWS |
RECENT PUBLICATION HIGHLIGHTS |
|---|---|
| Goldman Lab Touts Cardiovascular Student Research For Pfeiffer Foundation Visit CLICK HERE >> |
Ref J, Lefkowitz E, Anilkumar A, Acharya S, Grijalva A, Gorman G, Daugherty S, Fox K, Lancaster J, Acharya T, Moulton M, Avery R, and Goldman S. Regional Left Ventricular Wall Stress Post-Myocardial Infarction with Magnetic Resonance Imaging in Swine. American Journal of Physiology. Heart and Circulatory Physiology 2025 (In Press) |